GreyMatters
Educational articles, BetterBrain resources, latest in brain health, and news about us. Written for you, with expertise (and love).

Fighting Dementia with CBT: A proactive approach
Cognitive-behavioral therapy (CBT) has long been recognized as a powerful tool in managing mental health disorders, but its potential role in preventing dementia is only beginning to be appreciated1,2. There are two ways that CBT can help. First, CBT is a powerful tool which can combat anxiety, depression, and other mental health disorders, which increase the risk of dementia3,4. Second, CBT can be used to facilitate habit change - that is to say, help users adopt behaviors which promote brain health.
How does CBT work?
CBT is a structured form of psychotherapy that relies on the principle of identifying and changing certain thought patterns and behaviors. The underlying principle is that the brain is “plastic” or flexible throughout life, which means that we can shape the connections our brain makes. The therapy is collaborative, with the client and therapist working together to set goals and practice new skills. The specifics of a CBT session will vary depending on the needs of each individual, but sessions generally involve recognizing distorted thinking, challenging irrational beliefs, and developing healthier responses. CBT also encourages behavioral changes by gradually facing fears or engaging in positive activities.
CBT in Alzheimer’s prevention
Combating mental illness
Your mental health is closely linked to your brain health. Depression, anxiety, and other disorders can actually increase inflammatory stress in your brain and disrupt your cognitive function. There are several different approaches to treating mental illness, and CBT happens to be highly effective for some people.
Forming healthy habits
Much of dementia prevention relies on addressing known lifestyle risk factors, things like physical inactivity, poor diet, diabetes, and high blood pressure. Forming and maintaining healthy habits can feel challenging, but CBT can help facilitate behavior change and keep you on the right track.
Common CBT principles
Because CBT is a tool, many of its principles apply just as well to managing mental health as to improving lifestyle habits. Common techniques include:
- Awareness and Identification: CBT begins with helping individuals become more aware of their current state. What situations or thoughts trigger a negative cascade? Which of my habits aren’t the healthiest?
- Cognitive Restructuring: This is a fancy way of saying challenging negative thoughts. By examining negative emotions and thoughts, individuals can start to think about them objectively. For mental health, this can be changing “something catastrophic will happen” to “I can take on this challenge.” For habit formation, this may be replacing "changing my diet won’t make a difference" with "every healthy meal contributes to my resilience."
- Behavioral Experiments: CBT employs behavioral experiments to challenge negative beliefs and test out new behaviors in a controlled manner. This may look like gradually facing a feared situation, engaging in activities that carry a sense of accomplishment, or starting to exercise with 10-minute daily walks. The purpose here is to gain confidence and reinforce the challenge to negative thoughts with real-life actions.
- Goal Setting: Together with a therapist, individuals set specific, achievable goals related to their needs. These may be thing like developing problem-solving skills to improve their sense of control, or things like increasing weekly physical exertion. The most important thing is for these goals to feel realistic and manageable.
- Reinforcement: Positive changes are reinforced through self-monitoring and resilience techniques. Tracking change over time helps establish a feedback loop where improvement becomes a natural motivator, while practical skills for managing setbacks help sustain long-term behavior change.
By systematically working through these steps, CBT provides individuals with the tools and confidence to implement and sustain changes - many of which contribute to preventing dementia.
A strong tool for prevention
It’s important to recognize that CBT isn’t a silver bullet - it’s a tool that’s helped millions of people, and it requires conscious work to implement. With that said, the potential of CBT in preventing Alzheimer’s is vast. It not only helps address mental illness, but also incorporates lifestyle changes that tackle the physiological underpinnings of dementia. Implementing CBT strategies that promote healthy aging could be key in reducing the burden of dementia, emphasizing prevention over treatment and maintaining cognitive vitality well into the later years of life.
Resources on finding CBT providers
If you are interested in trying CBT, there’s several ways to get started.
- Online directories and telehealth platforms can help you find a professional to work with. You can often find therapists through your insurance plan or your employee benefits, or through listing websites like Zocdoc or Psychology Today. You can also look on telehealth platforms like Talkspace or Betterhelp, though not all of these accept insurance.
- Community health centers often also provide CBT services. These are typically available at reduced rates, and focus primarily on mental health.
- Books can help you learn more about CBT and its practice. Feeling Great: The revolutionary new treatment for depression and anxiety is a widely praised book by Dr. David Burns, a psychiatrist and professor of Psychiatry at Stanford.

Clearing the Air: How Pollution Influences Alzheimer's Risk
When you think of air pollution, respiratory disease is usually the first thing to come to mind. However, recent findings from the Emory Healthy Brain Study1 has begun to show that long-term exposure to tiny particles called PM2.5 has been associated with the accumulation of amyloid plaques in the brain, which is a hallmark of Alzheimer's disease. While this doesn't prove that PM2.5 exposure leads to Alzheimer's, it suggests a potentially elevated risk, especially among those exposed to poor quality air over longer periods of time.
Air quality is typically measured by the amount of specific pollutants in the air. The Emory Healthy Brain Study looked at a type of pollutant called PM2.5, which is fine particulate matter with a diameter of less than 2.5 micrometers (about 30 times smaller than a human hair). These particles are so fine they can bypass the body's airway defenses and enter the bloodstream. Common sources of PM2.5 include vehicle emissions, industrial combustion, and natural occurrences like wildfires. Because the particles can enter the bloodstream, they can cause health issues that go beyond simple respiratory irritation, potentially affecting brain health and contributing to cognitive decline.
Key Findings from the Study
- Increased PM2.5 exposure is associated with worse results on Alzheimer’s pathology biomarkers: The study indicated that higher levels of PM2.5 exposure over one and three years are associated with lower concentrations of amyloid-beta 42 (Aβ42) in cerebrospinal fluid (CSF). Aβ42 is a biomarker whose decreased levels suggest an accumulation of amyloid plaques in the brain, which is a hallmark of Alzheimer’s dementia.
- Specific Focus on Traffic-Related PM2.5: While the study looked at both ambient (general environmental) and traffic-related PM2.5, the findings were particularly noteworthy for ambient PM2.5. This suggests that while traffic contributes significantly to PM2.5 levels, other sources of pollution also play a crucial role in influencing Alzheimer’s disease biomarkers.
- Implications for Alzheimer’s Risk: The research underscores that even PM2.5 below levels currently considered risky by environmental standards, there is a tangible increase in the risk of developing Alzheimer’s disease. This calls for a reassessment of what is considered “safe” exposure to PM2.5, particularly for populations at risk of Alzheimer’s.
Reducing Exposure
Individuals living in high pollution areas can reduce their exposure by:
- Using air purifiers at home
- Avoiding outdoor activities when pollution levels are high
- Supporting clean air initiatives aimed at reducing emissions
Conclusion
The findings from Emory University’s research are a vital addition to our understanding of environmental factors in Alzheimer’s disease risk. They not only highlight the need for stricter air pollution controls but also suggest that everyday actions to reduce exposure to PM2.5 could be a feasible strategy for Alzheimer's prevention. As we continue to uncover more about the impact of our environment on health, it becomes increasingly clear that tackling air pollution is not just about preserving our planet—it's also about protecting our minds.

Saunas and Alzheimer's: Hot Topic or Just Hot Air?
For centuries, saunas have been lauded for their supposed health benefits, from improved cardiovascular function to detoxification. The recent trends around longevity seem to have revitalized the use of saunas, now considered a popular "health hack". But could spending time in these heated chambers also benefit your brain? Recent research suggests that sauna use might indeed play a role in mitigating the risk of Alzheimer's disease. In this article, we'll explore the scientific evidence behind this claim and consider how sauna use may impact your brain health.
The Connection Between Saunas and Alzheimer's Disease
The Finnish Study
A study from Finland has brought attention to the potential benefits of saunas for brain health. According to the 2,315 person study1, men who used a sauna 4-7 times a week showed a 65% reduced risk of Alzheimer's disease compared to those who used it once a week. Although the study mainly focused on men and thus requires further exploration for generalization, the findings are promising - 65% is a staggering number. If true, this would imply we could cut Alzheimer's prevalence from 6 million to 2 million in the US if only everyone used the sauna daily!
The Underlying Mechanisms
Scientists have proposed several mechanisms through which saunas may benefit the brain. One suggestion is that saunas can significantly improve sleep quality and time in deep sleep, which improves the brain's ability to clear toxic proteins. Moreover, heat stress activates heat shock proteins that can repair damaged proteins, which may play a role in neurodegenerative diseases like Alzheimer's. Lastly, saunas may improve various markers of vascular function, such as blood pressure and blood circulation, known risk factors for Alzheimer's.
Caveats and Considerations
First, the impact was more muted for those who used the sauna only 2-3 times a week (~22% risk reduction). Additionally, while the Finnish study shows a correlation, and certainly attempted to control for relevant variables, it is always very challenging to prove causation in retrospective studies.
Conclusion
The notion that saunas could "incinerate" your Alzheimer's risk is captivating, they should not be viewed as a standalone solution. While promising studies hint at a beneficial correlation, saunas are not a guaranteed prevention method for Alzheimer's. However, given their other health benefits and the intriguing data suggesting a potential role in brain health, saunas could be a worthwhile addition to your wellness routine. Plus, who doesn't enjoy an intense sauna session followed by a cold plunge or shower?

Why Is Alzheimer's More Common in Women?
When it comes to Alzheimer's disease, gender plays an undeniable role. A staggering two-thirds of those diagnosed with Alzheimer's in the United States are women. This disparity has puzzled researchers for years. Initially, many attributed it to the longer lifespan of women compared to men. However, as our understanding of the disease deepens, we've learned that longevity alone doesn't fully explain the 2X difference in prevalence.
The Longevity Theory Falls Short
For a long time, the prevailing explanation for why more women than men were diagnosed with Alzheimer's was simple: women live longer, and Alzheimer's is a disease that primarily affects older adults. However, this explanation has increasingly come under scrutiny. As it turns out, the difference in lifespan between men and women isn't sufficient to account for the wide gap in Alzheimer's cases. The narrative is much more nuanced and involves a complex interplay of biological and social factors.
The Menopause Transition Hypothesis
Menopause is a significant biological milestone in a woman's life, marked by the end of menstrual cycles and fertile years. One of the most significant changes that accompany menopause is a decline in estrogen levels. Estrogen is not just a reproductive hormone; it also has protective effects on the brain. The sharp decrease in estrogen during the menopause transition has been hypothesized to elevate the risk of Alzheimer's among women. In fact, cognitive decline associated with reduced estrogen levels has been reported, especially during the peri-menopausal and post-menopausal phases.
A beacon of hope: Hormone Replacement Therapy (HRT)
Given the hypothesized link between menopause and Alzheimer's risk, Hormone Replacement Therapy (HRT) has been studied as a potential preventive measure. Some evidence indicates that HRT could mitigate the risk of Alzheimer's among post-menopausal women. One prospective study1in particular demonstrated a 41% reduction in the risk of Alzheimer's in women who did HRT vs those who did not. Of course, any decision to start HRT should be made through a physician who can account for all contraindications.
The Often Overlooked Role of Caregiving
The gender disparity in Alzheimer's doesn't end with disease prevalence; it also manifests in caregiving. Women make up a significant majority of Alzheimer's caregivers, often bearing the emotional and physical burden of caring for afflicted family members. This role can lead to heightened stress levels, which in turn could potentially impact a woman’s own cognitive health.
Conclusion
The question of why Alzheimer's disproportionately affects women is far from straightforward. While the longevity theory has been partially debunked, the menopause transition and its hormonal changes offer a compelling avenue for understanding the gender disparity in Alzheimer's prevalence. Even social factors like caregiving roles cannot be discounted. Understanding these contributing factors can pave the way for gender-specific preventive strategies, which are beginning to be implemented in clinical practice.

Should you get tested for APOE4?
Chance are, you know someone who has tested for their APOE genotype. With the advent of consumer genotyping companies such as 23andme, genetic testing for Alzheimer's risk has become increasingly accessible, with the APOE4 gene variant taking center stage in the discussion. The question that many people are asking is: Should I get tested for APOE4? This article aims to provide a balanced perspective, detailing the pros and cons to help you make an informed decision.
What Is APOE4?
The APOE gene produces a protein essential for fat metabolism and is involved in brain cell repair. There are three main variants of this gene—APOE2, APOE3, and APOE4—with the APOE4 variant being strongly associated with an increased risk of developing Alzheimer's disease. While having this gene variant doesn't guarantee that you'll develop Alzheimer's, it can significantly elevate your risk. 20-25% of people have 1 copy of APOE4, conferring a 2-3X increase in Alzheimer's risk, while 2-3% of people have 2 copies, which implies an 8-10X increase in risk.
Advantages of APOE4 Testing
Empowers You to Make Informed Choices
Perhaps the most compelling reason for getting tested is the ability to make informed decisions about your health. There are specific recommendations for those carrying APOE4 such as significantly increasing DHA consumption given impaired absorption. Additionally, research suggests that APOE4 carriers get even more benefit from a range of interventions than non-carriers. In fact, some experts suggest that by applying the right interventions, you can completely mitigate the impact of having a copy of APOE4.
Opens opportunities for clinical trials and futures therapies
There is a significant research focus on APOE4 and potential pharmacological approaches to mitigating the associated risk. Testing may open up avenues for participating in such trials. Furthermore, as therapies get approved in the future for APOE4 carriers, you'll be well positioned to take advantage.
Offers Information for Family Planning
Your genetic makeup doesn't just affect you; it could also be informative for your family members. Given the heritability of the gene, knowing that you carry the APOE4 variant could give valuable insights into your relatives such as parents who may be at higher risk for developing dementia.
Drawbacks of APOE4 Testing
Carries Emotional and Psychological Weight
Although APOE4 is simply a risk factor and is far from being deterministic, finding out that you're at higher risk for Alzheimer's can be emotionally taxing. While the REVEAL study1 showed that disclosing ApoE4 status did not cause clinically significant anxiety or depression after 6 month follow up, responses are of course very individualized. Before taking the test, consider whether you're emotionally prepared for the results.
Doesn't Guarantee Prevention or Cure
At present, there is no cure for Alzheimer's. Knowing you have the APOE4 gene can offer a sense of urgency to adopt preventive measures, but it doesn't guarantee that you'll be able to ward off the disease.
Raises Ethical and Privacy Concerns
Genetic testing often brings up privacy issues. There's always the risk of data leaks or misuse by third parties, including insurance companies, even though laws exist to prevent genetic discrimination (e.g., GINA for health insurance). Be aware of these concerns when contemplating testing.
The Decision is Yours to Make
Choosing whether to undergo APOE4 testing is a deeply personal decision that should be based on multiple factors, including your emotional readiness, family history, and the current state of your cognitive health. Regardless of your decision, remember that the genetics are just one piece of a very complicated puzzle.
The Rise of Amyloid Blood Tests
The Landscape of Alzheimer's Biomarkers
When it comes to assessing the risk of cardiovascular disease, we have straightforward biomarkers such as ApoB (LDL) and blood pressure which can predict risk fairly accurately. However, the realm of neurodegenerative diseases like Alzheimer's is a lot more messy. For years, researchers and clinicians have depended PET scans or cerebral spinal fluid (CSF) for analyzing biomarkers like amyloid and tau proteins. But these procedures are expensive ($5-10K in the case of PET) or invasive (CSF requires a lumbar puncture), making them impractical for widespread use.
Enter blood amyloid tests, a relatively new but promising diagnostic aimed at solving this problem.
What Are Blood Amyloid Tests and How Do They Work?
As the name suggests, these tests measure the concentration of various amyloid beta proteins in the blood (and sometimes tau as well) as a proxy for amyloid deposition in the brain. While the scientific community continues to debate whether amyloid pathology is a root cause of Alzheimer's disease or merely a symptom of other underlying brain pathologies, there is a clear association between the extent of amyloid presence in the brain and the manifestation of the disease.
One of the original commercially available tests was PrecivityAD by C2N. This test needs to be ordered by a physician and was designed to predict the likelihood of Alzheimer's Disease (AD) pathology by analyzing a few key factors:
- The ratio of two variants of amyloid beta proteins, specifically amyloid beta 42 and amyloid beta 40
- The ApoE variant of the patient
- The age of the individual
By amalgamating these variables, the test attempts to gauge the probability of a positive PET scan. While it's too early to draw any definitive conclusions, there are two primary reasons why looking at this data could be valuable:
- Comprehensive Risk Assessment: The test results can be used in combination with other factors like family history, genetics, metabolic health, vascular health and cognitive testing to assess the overall risk.
- Monitoring Interventions: The score could be used as a dynamic indicator to monitor the effectiveness of steps taken to mitigate Alzheimer's risk. If the score decreases, it suggests that the ratio of amyloid beta 42 to amyloid beta 40 has changed favorably and thus risk has been reduced.
Since then, C2N launched a second generation version of the tests, PrecivityAD21, which accounts for serum tau concentration for additional accuracy. In August of 2023, Quest launched a direct-to-consumer version of the test that does not require physician ordering. While the test is not quite as accurate as C2N in predicting a positive PET, it comes at a materially lower cost - $400 as of the date of this writing.
Applicability: Who Should Consider blood amyloid tests?
According to medical experts, the test should be reserved for those at high risk of developing Alzheimer's, as its sensitivity and specificity are still not entirely understood. The key term here is "pre-test probability." The higher the pre-test probability, the more reliable the test becomes in predicting a positive or negative outcome.
Final Thoughts
The emergence of amyloid (and tau) blood tests is an exciting development in the field of Alzheimer's research and prevention. Although not a complete solution, they do provide an additional layer of information that can potentially enhance our ability to serve people at risk of developing disease. As our grasp of amyloid biomarkers improves, these tests could become integral parts of a broader, more nuanced approach to diagnosis and risk assessment.
Update April 19, 2024
Roche, in collaboration with Eli Lilly, has launched the Elecsys pTau-2172 blood test, which has recently received breakthrough device designation from the FDA. This means it was recognized as an effective tool for diagnosis, and is a critical milestone in how we identify Alzheimer's Disease. This test targets the tau protein pTau-217 and has the unique ability to distinguish AD from other neurodegenerative diseases. This is particularly important given that clinical AD diagnoses often lack sensitivity and specificity. It’s all the more since over half of patients with cognitive impairment remain undiagnosed or incorrectly diagnosed. This advancement promises to enhance early diagnostic accuracy and significantly improve intervention strategies for AD, particularly as global dementia figures are projected to rise sharply by 2050. pTau-217 is now available as an add-on service with BetterBrain.
Get immediate insights with a 3 minute assessment
Start nowDietary Defenders: Prebiotic Fibers in Alzheimer's Prevention
As Alzheimer's disease continues to impact millions globally, the scientific community is increasingly focusing on the gut-brain axis. This complex communication network, which links the gastrointestinal tract and the brain, could play a major role in preventing cognitive decline. Recent discoveries1 have shown that gut microbiota might affect everything from brain development to behavior to disease states, and researchers are starting to explore how the gut-brain axis can influence dementia risk.
Exploratory study: A closer look at fiber's impact on aging brains
The School of Life Course & Population Sciences at King’s College London spearheaded a pivotal double-blind study2 (the same type of study as used for clinical trials) with participants over 60 years old. Their research aimed to uncover the cognitive effects of consuming prebiotic fibers compared to a placebo.
Fiber fuels cognitive fortitude
Like any organism, the components making up the gut microbiome need food to survive. One source of nutrients for them is prebiotic fibers, such as inulin and fructooligosaccharides (FOS), both of which were the focus of the King’s College study. The researchers found that participants who took prebiotic supplements had more of one species of healthy bacteria called Bifidobacterium in their gut. This species has previously been linked to better cognitive performance, and indeed the participants who took supplements showed improved cognitive function scores through the same memory tests that are used as an early indicator of Alzheimer’s disease.
Why is this happening?
The composition of the gut microbiome has drastically changed over human history. Advances in agriculture, industrialization and globalization may have caused a decrease in gut microbial diversity, which has been associated with worse health outcomes. In particular, a review of multiple studies1 suggests that changes in the microbiome can lead to behavioral changes. In another study3 comparing 25 patients diagnosed with Alheimer’s disease to 25 healthy individuals, those with Alzheimer’s were found to have reduced gut microbial diversity.
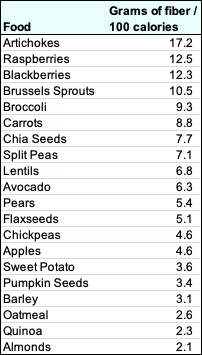
Keeping an eye on your intake
Let’s get specific. Women should aim to consume 21-25g of fiber per day. Men should aim for 30-38g4. Here is a list of some common fiber-dense foods to consider adding into your diet.
A promising path to cognitive health
Emerging evidence connecting dietary habits, gut microbiota, and brain function highlights a novel approach to combat Alzheimer’s disease. The gut-brain axis is still a new area of research - there is much we don’t know, and many researchers around the world are investigating the different ways in which the microbiome influences our brain health. Such studies not only pave the way for innovative therapeutic avenues but also emphasize the profound impact our diet can have on mental and overall health.
Putting the science in action
- Eat enough fiber each day to make sure you are nourishing your gut microbiome. Women should strive for 21-25g daily, while men should aim for 30-38g.
- Learn more about the importance of your gut health on your brain and body through the Peter Attia Drive podcast.some text
- Episode #215 goes in-depth on the GI system - skip to 34:30 for ways in which the gut and brain communicate, and to 1:55:00 for ways to promote your gut microbiome using your nutrition.
- Episode #283 discusses the microbiome specifically - learn more about the importance of fiber at 38:30 and about the gut-brain axis at 50:15.
The Role of Homocysteine in Dementia Risk
Homocysteine is a naturally occurring amino acid in our body and can spike acutely, such as after staying up all night. In healthy people, homocysteine naturally clears over time. However, at chronic high concentrations, it is associated with various health issues, including heart disease and, notably, cognitive decline. In fact, having blood homocysteine levels over 14 μmol/L is associated with a nearly doubled risk of dementia1. Luckily, there are simple ways to lower your homocysteine levels - most notably B vitamin supplementation.
Brain Atrophy, Aging and Cognitive Decline
As we age, our brains naturally undergo some amount of atrophy, or decrease in size, which involves a loss of neurons and their connections. This process is accelerated in Alzheimer’s dementia2. With a lower brain volume and fewer neural connections, it’s easy to see how atrophy can lead to lasting cognitive impairment. One factor that has a strong influence on the rate of brain atrophy is blood concentration of homocysteine. Several studies3,4 link elevated homocysteine levels are linked with a heightened risk of dementia.
The role of B vitamins
You won’t often hear us say this, but you have an ace up your sleeve in fighting homocysteine: B vitamins. One study2 investigated the effects of using B6, B9, and B12 vitamins over the course of two years, using the same level of rigor that is commonly used for drug clinical trials.
On average, people who used B vitamins lowered their overall homocysteine levels by 32% and experienced a 30% slower rate of brain atrophy. In fact, those who started with very high levels of blood homocysteine (> 14 μmol/L) managed to slow their atrophy rate by 53%. In other words, this study suggests that the simple act of taking a daily B vitamin supplement can cut your dementia risk in half.
The type of B vitamin matters
There are two factors to consider when selecting a B vitamin supplement. The first is what vitamins you are getting. The study mentioned above specifically tested the use of vitamins B6, B9 (also known as folate), and B12. It’s important to get a mix of both. The second is whether or not you select the methylated form of the vitamins. Methylation is a biological process that makes the vitamins more available for your body to use. In other words, the same dose of methyl-B vitamins will be more strongly absorbed than normal B vitamins. This is especially important for people with mutations in the MTHFR gene, since they otherwise have trouble absorbing B vitamins. We generally recommend taking methylated B vitamins since they are perfectly safe, but if you are sensitive to overmethylation, you may want to consider regular B vitamins to avoid side effects like headaches, anxiety, or irritability.
Broader Implications for Dementia Prevention
Homocysteine is a critically important risk factor for dementia. Not only does it accelerate brain atrophy, it also aggravates other conditions through inflammation and oxidative stress. Thankfully, B vitamins are an extremely effective tool to lower homocysteine levels. While there are many other ways of managing your homocysteine levels, most notably through diet, exercise, and stress management, B vitamins are a low-effort high-impact way to keep your brain atrophy at bay.
Get started on managing your homocysteine
- Measure your blood homocysteine levels to learn where you stand. Homocysteine is one of the 50+ biomarkers tested during your BetterBrain Essentials blood draw.
- Consider using B vitamin supplements to lower your homocysteine, ideally below 9 μmol/L. We recommend Pure Encapsulations MethylAssist, but make sure you use an unmethylated alternative if you are sensitive to overmethylation.
- Learn more about homocysteine on the Peter Attia Drive episode on dementia. This episode covers many topics, so if you’re just interested in homocystine, skip ahead to 1:09:00.
Clearing the Air: How Pollution Influences Alzheimer's Risk
When you think of air pollution, respiratory disease is usually the first thing to come to mind. However, recent findings from the Emory Healthy Brain Study1 has begun to show that long-term exposure to tiny particles called PM2.5 has been associated with the accumulation of amyloid plaques in the brain, which is a hallmark of Alzheimer's disease. While this doesn't prove that PM2.5 exposure leads to Alzheimer's, it suggests a potentially elevated risk, especially among those exposed to poor quality air over longer periods of time.
Air quality is typically measured by the amount of specific pollutants in the air. The Emory Healthy Brain Study looked at a type of pollutant called PM2.5, which is fine particulate matter with a diameter of less than 2.5 micrometers (about 30 times smaller than a human hair). These particles are so fine they can bypass the body's airway defenses and enter the bloodstream. Common sources of PM2.5 include vehicle emissions, industrial combustion, and natural occurrences like wildfires. Because the particles can enter the bloodstream, they can cause health issues that go beyond simple respiratory irritation, potentially affecting brain health and contributing to cognitive decline.
Key Findings from the Study
- Increased PM2.5 exposure is associated with worse results on Alzheimer’s pathology biomarkers: The study indicated that higher levels of PM2.5 exposure over one and three years are associated with lower concentrations of amyloid-beta 42 (Aβ42) in cerebrospinal fluid (CSF). Aβ42 is a biomarker whose decreased levels suggest an accumulation of amyloid plaques in the brain, which is a hallmark of Alzheimer’s dementia.
- Specific Focus on Traffic-Related PM2.5: While the study looked at both ambient (general environmental) and traffic-related PM2.5, the findings were particularly noteworthy for ambient PM2.5. This suggests that while traffic contributes significantly to PM2.5 levels, other sources of pollution also play a crucial role in influencing Alzheimer’s disease biomarkers.
- Implications for Alzheimer’s Risk: The research underscores that even PM2.5 below levels currently considered risky by environmental standards, there is a tangible increase in the risk of developing Alzheimer’s disease. This calls for a reassessment of what is considered “safe” exposure to PM2.5, particularly for populations at risk of Alzheimer’s.
Reducing Exposure
Individuals living in high pollution areas can reduce their exposure by:
- Using air purifiers at home
- Avoiding outdoor activities when pollution levels are high
- Supporting clean air initiatives aimed at reducing emissions
Conclusion
The findings from Emory University’s research are a vital addition to our understanding of environmental factors in Alzheimer’s disease risk. They not only highlight the need for stricter air pollution controls but also suggest that everyday actions to reduce exposure to PM2.5 could be a feasible strategy for Alzheimer's prevention. As we continue to uncover more about the impact of our environment on health, it becomes increasingly clear that tackling air pollution is not just about preserving our planet—it's also about protecting our minds.
Fighting Dementia with CBT: A proactive approach
Cognitive-behavioral therapy (CBT) has long been recognized as a powerful tool in managing mental health disorders, but its potential role in preventing dementia is only beginning to be appreciated1,2. There are two ways that CBT can help. First, CBT is a powerful tool which can combat anxiety, depression, and other mental health disorders, which increase the risk of dementia3,4. Second, CBT can be used to facilitate habit change - that is to say, help users adopt behaviors which promote brain health.
How does CBT work?
CBT is a structured form of psychotherapy that relies on the principle of identifying and changing certain thought patterns and behaviors. The underlying principle is that the brain is “plastic” or flexible throughout life, which means that we can shape the connections our brain makes. The therapy is collaborative, with the client and therapist working together to set goals and practice new skills. The specifics of a CBT session will vary depending on the needs of each individual, but sessions generally involve recognizing distorted thinking, challenging irrational beliefs, and developing healthier responses. CBT also encourages behavioral changes by gradually facing fears or engaging in positive activities.
CBT in Alzheimer’s prevention
Combating mental illness
Your mental health is closely linked to your brain health. Depression, anxiety, and other disorders can actually increase inflammatory stress in your brain and disrupt your cognitive function. There are several different approaches to treating mental illness, and CBT happens to be highly effective for some people.
Forming healthy habits
Much of dementia prevention relies on addressing known lifestyle risk factors, things like physical inactivity, poor diet, diabetes, and high blood pressure. Forming and maintaining healthy habits can feel challenging, but CBT can help facilitate behavior change and keep you on the right track.
Common CBT principles
Because CBT is a tool, many of its principles apply just as well to managing mental health as to improving lifestyle habits. Common techniques include:
- Awareness and Identification: CBT begins with helping individuals become more aware of their current state. What situations or thoughts trigger a negative cascade? Which of my habits aren’t the healthiest?
- Cognitive Restructuring: This is a fancy way of saying challenging negative thoughts. By examining negative emotions and thoughts, individuals can start to think about them objectively. For mental health, this can be changing “something catastrophic will happen” to “I can take on this challenge.” For habit formation, this may be replacing "changing my diet won’t make a difference" with "every healthy meal contributes to my resilience."
- Behavioral Experiments: CBT employs behavioral experiments to challenge negative beliefs and test out new behaviors in a controlled manner. This may look like gradually facing a feared situation, engaging in activities that carry a sense of accomplishment, or starting to exercise with 10-minute daily walks. The purpose here is to gain confidence and reinforce the challenge to negative thoughts with real-life actions.
- Goal Setting: Together with a therapist, individuals set specific, achievable goals related to their needs. These may be thing like developing problem-solving skills to improve their sense of control, or things like increasing weekly physical exertion. The most important thing is for these goals to feel realistic and manageable.
- Reinforcement: Positive changes are reinforced through self-monitoring and resilience techniques. Tracking change over time helps establish a feedback loop where improvement becomes a natural motivator, while practical skills for managing setbacks help sustain long-term behavior change.
By systematically working through these steps, CBT provides individuals with the tools and confidence to implement and sustain changes - many of which contribute to preventing dementia.
A strong tool for prevention
It’s important to recognize that CBT isn’t a silver bullet - it’s a tool that’s helped millions of people, and it requires conscious work to implement. With that said, the potential of CBT in preventing Alzheimer’s is vast. It not only helps address mental illness, but also incorporates lifestyle changes that tackle the physiological underpinnings of dementia. Implementing CBT strategies that promote healthy aging could be key in reducing the burden of dementia, emphasizing prevention over treatment and maintaining cognitive vitality well into the later years of life.
Resources on finding CBT providers
If you are interested in trying CBT, there’s several ways to get started.
- Online directories and telehealth platforms can help you find a professional to work with. You can often find therapists through your insurance plan or your employee benefits, or through listing websites like Zocdoc or Psychology Today. You can also look on telehealth platforms like Talkspace or Betterhelp, though not all of these accept insurance.
- Community health centers often also provide CBT services. These are typically available at reduced rates, and focus primarily on mental health.
- Books can help you learn more about CBT and its practice. Feeling Great: The revolutionary new treatment for depression and anxiety is a widely praised book by Dr. David Burns, a psychiatrist and professor of Psychiatry at Stanford.
Harnessing Heart Rate Variability for Brain Health
The intricate dance between our heart rate and brain function is more influential than we might think. Recent studies reveal that heart rate variability (HRV)—the measure of variations between individual heartbeats—affects our brain health, decision-making abilities, and even our emotional regulation. HRV is a physiological metric that we can train ourselves to improve, and its connections to the brain make HRV training a promising technique for dementia prevention and enhancing cognitive function.
Understanding the Heart-Brain Connection:
While your heart rate is the average number of beats per minute, HRV is the difference in length between individual heartbeats.

HRV is not just a measure of heart health - it reflects the health and balance of the autonomic nervous system (ANS), which is responsible for involuntary body functions. In particular, HRV serves as a key indicator of the interaction between the two components of the ANS: the sympathetic (fight or flight) and parasympathetic (rest and digest) nervous systems. Interestingly, there is a two-way feedback system between these nervous systems and the heart. The signals from the sympathetic and parasympathetic influence heart rate, and heart rate regulates the balance of these two systems. By exerting an influence on the ANS, heart rate variability helps regulate emotions and stress responses. In general, higher HRV is associated with better control over decision-making processes, emotional responses, anxiety, and social behaviors1.
Booting your HRV
Common HRV training protocols call for biofeedback, which is a fancy way of saying you need a sensor to measure your heart rate variability so you can improve it. HRV training involves guided exercises such as paced breathing while looking at real-time heart rate data to learn to consciously control heart rate variability. This is what makes it different from techniques like yoga or meditation - their focus is commonly to achieve a balanced state, whereas the goal of HRV training is to modulate physiological responses.
This technique not only promotes a balanced state but also has long-lasting effects on both mental and physical health. Thanks to the heart-brain connection, HRV training leads to improved emotional regulation and stress management. Although different training regimens exist, just five minutes of HRV training twice a day can significantly enhance control over the heart and reduce anxiety levels during stressful periods2. Critically, the benefits of HRV training extend far beyond mood and feeling: they also correlate with enhanced executive functions like planning, problem-solving, and resisting unhealthy impulses1. In fact, the benefits of this training can persist, with improvements seen even 12 weeks after stopping the training1.
Tying back to dementia
Thanks to its influence on stress response, cognitive function, healthy behaviors, and cardiac health, it’s no surprise that higher HRV is associated with stronger resilience against cognitive decline2,3. Since the simple daily practice of HRV biofeedback training can improve your HRV, we can think of it as a valuable tool to help delay the onset and progression of dementia. It's a clear testament to the power of our bodies' interconnected systems, and a reminder that taking care of our heart is as much about our mind.
Where to start with HRV training
- Choose a tracking device: the first step is to make sure you have the right equipment to measure your heart rate variability. Because you are measuring the time between individual heartbeats, you need a particularly sensitive device. Although some common wearables like the Apple watch or Whoop claim to measure HRV, it’s better to opt for a specialized chest strap like the Polar H10 which can connect to your other wearables.
- Visualize your data: once you have a solid device, use an app like Elite HRV or Welltory (both of which have a free version available) so that you can visualize your HRV in real time. These apps also come with a wealth of additional insights that can help you fine tune your training.
- Start training: you can find guided training sessions either through apps like Elite HRV or through online courses provided by organizations like the HeartMath Institute. YouTube also has a number of guided HRV routines you can try, such as this one from the Huberman Lab show.
- Learn more: The Peter Attia Drive podcast has an episode that dives deep into HRV so you can learn more about how it works and how it can help you.
Metabolic Syndrome as a Gateway to Dementia
It’s a well-known fact that Alzheimer’s disease is closely linked to metabolic health, to the point that some experts have begun to refer to it as Type III Diabetes. But what many people don’t know is that poor metabolic health is a strong risk factor for dementia long before it progresses to diabetes, even for people without a family history.
Decoding metabolic syndrome
Before you get diagnosed with diabetes, your body goes through a number of changes. Cells in your body become desensitized to insulin, which usually tells them to absorb sugar from your bloodstream. This results in chronically elevated blood sugar and in turn starts causing problems for your heart, liver, brain, and other organs. This pre-diabetic phase is called metabolic syndrome, and it affects ~25% of adults worldwide, including 40% adults aged 60+ in the U.S. Most of them do not know that metabolic syndrome is a health risk.
Metabolic syndrome is diagnosed when an individual has three or more of the following:
- High triglycerides (≥150 mg/dL)
- Elevated blood pressure (≥130 mmHg systolic or ≥85 mmHg diastolic) OR use of antihypertensive medication
- High fasting glucose (≥100 mg/dL OR use of glucose lowering medications)
- Low HDL cholesterol (<40 mg/dL in men; <50 mg/dL in women OR use of lipid-modifying medication)
- Abdominal obesity (waist circumference ≥102 cm for men and ≥88 cm for women)
It’s worth noting that hemoglobin A1c (HbA1c), a common marker for diabetes, does not feature on this list. Although a doctor won’t use A1c to diagnose metabolic syndrome, it’s still an important marker to keep track of your metabolic health.
Connecting metabolic syndrome to brain health
A large retrospective study1 analyzed data from 175,000 participants over a period of 15 years. Participants were aged 60+ and represented a variety of sociodemographic, lifestyle, and genetic backgrounds. With regards to the metabolic syndrome diagnosis criteria listed above, the study found that:
- Having three conditions increases dementia risk 12%
- Having four to five conditions is associated with an even stronger risk
- The link between metabolic syndrome and dementia is particularly strong in individuals who do not carry the APOE ε4 allele (typically, these are individuals with a lower risk of dementia)
Taking action
The first step is to know where you stand. It’s important to establish a baseline by measuring metabolic markers in your blood and potentially using a continuous glucose monitor (CGM) to see how your blood sugar reacts to your daily habits. This will help you make an informed decision on how to approach your metabolic health.
Metabolic health is strongly tied to your lifestyle - particularly your diet, physical activity, and sleep. There’s also several different drugs, like statins or ACE inhibitors, available to help manage symptoms. However, this post isn’t meant to serve as a meal plan or exercise sheet. Instead, we’ve put together a list of hacks that we think can make a difference even if you haven’t fully optimized your health.
- Drink a tablespoon of vinegar ~20 minutes before a meal. This helps avoid spikes in your blood sugar.
- Go for a walk after meals, especially if those meals are heavy on carbs (e.g., pasta, potatoes, bread). This helps your muscles absorb glucose more efficiently.
- Perform at least 10m of vigorous exercise per day. Raising your heart rate (e.g., through a short HIIT session) helps boost your insulin sensitivity, which keeps blood sugar low.some text
- Exercise is most effective at reducing blood sugar spikes when done within an hour before or after a meal
- Eat your carbs last. Start your meal by eating vegetables (which are high in fiber), then eating proteins and fats, and finally moving to carbs. This helps slow the absorption of sugar into your bloodstream, and in turn reduce sugar spikes.
Small steps add up
Although the hacks mentioned above aren’t meant to replace a healthy lifestyle, they can help you make an immediate improvement in your metabolic health and kickstart your dementia prevention efforts. Remember - working on your metabolic health isn’t just about preventing diabetes, it’s about safeguarding your cognitive health.
Actions to consider
- Measure your metabolic markers. Some of these you may get on your annual physical (e.g., HbA1c, HDL-C, LDL-C, glucose, triglycerides, insulin). Others are less common (e.g., Lp(a), ApoB). Most importantly, don’t settle for just ok. These markers are worth optimizing. All the tests mentioned above are part of the 50+ biomarkers tested during your BetterBrain Essentials blood draw.
- Consider using a CGM to get a more accurate view of how your body processes sugar. Using a CGM, you can observe the effects of what you eat and your lifestyle on your blood sugar in real time, which can help inform the daily choices you make. We love the Dexcom G7, which may be challenging to buy over-the-counter but can be bought for cheaper through Signos.
- Learn more about homocysteine on the Peter Attia Drive podcast #252. This episode covers a wide variety of topics related to brain health, and links many different risks and possible interventions to metabolic health.

.png)